When you have acne, you want the best acne treatments that work quickly to resolve blemishes and prevent scarring. As a doctor I recommend using washes and soap substitutes, benzoyl peroxide, nicotinamide, salicylic acid, tea tree oil products or light therapy for home use. These usually solve acne within a few weeks, but you need to persevere with treatment as it takes time for the inflammation to resolve. If these don’t solve the acne within two months, then prescription treatments such as antibiotics, tretinoin or cosmetic therapies are available. I’ve reviewed the effectiveness of these different approaches below to help you select the best acne treatments that work. There is also a link between diet and acne.
What causes acne?
![]()
Quick link: These are the acne treatments I recommend from Boots, Amazon.co.uk andAmazon.com.
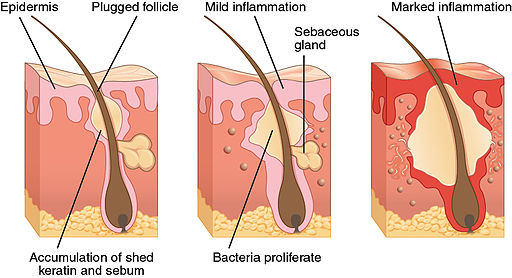
Acne occurs when blocked hair follicles become infected. Each hair follicle is associated with a sebaceous gland which secretes a conditioning oil (sebum). This oil normally travels along a narrow duct to reach the skin surface and helps keep your hair sleek and waterproof.
During adolescence, these oil glands become more activate under the influence of androgen hormones (especially dihydrotestosterone) and temporarily secrete increased amounts of oil, although this usually settles down with time.
The same hormones that stimulate increased oil production also stimulate increased division of cells within the ducts of the oil glands. These rapidly dividing cells tend to stick together, rather than being shed, and hair follicles become blocked. This traps the skin oil to form a classic, enlarging comedones (blackheads and whiteheads).
 As males have higher levels of androgen hormones than females, they are more likely to suffer from acne, and to have more severe symptoms.
As males have higher levels of androgen hormones than females, they are more likely to suffer from acne, and to have more severe symptoms.
In some women, acne is associated with polycystic ovary syndrome (PCOS) in hich sensitivity to androgen hormones is increased. Some women who do not have full-blown PCOS may also have sebaceous glands that are unusually sensitive to normal androgen levels. As a result, a flare-up of spots can be triggered by hormonal fluctuations associated with the second half of the menstrual cycle, menstruation, starting or stopping hormonal methods of contraception, or by pregnancy.
Female oestrogen levels fall as the menopause approaches, and this can increase the relative effects of circulating androgens to cause outbreaks of spots, although these are not usually so severe.
Acne and blackheads
A comedo is a blocked skin pore that forms a small bump, often on the forehead, nose and chin – the so-called oily T-zone of the face. When the blocked pore remains open, the trapped oil inside darkens (oxidises) on exposure to air to form a blackhead. Dissolved skin pigment (melanin) may darken it further – it is not trapped dirt as is commonly believed. Open blackheads can be unsightly, but they don’t usually progress to form spots unless they are squeezed. It is vitally important that you don’t pinch or squeeze blackheads or spots – however tempting – as this forces bacteria and inflammatory chemicals into surrounding tissues. The result is a spreading infection, with longer-lasting pimples that are larger and more likely to scar.
Acne and whiteheads
Closed comedones, whose ducts are totally blocked and covered with skin cells, are the ones that tend to explode into spots. Excess oil causes changes in skin acidity, which encourages colonisation with bacteria such as Propionibacterium acnes and Staphylococcus aureus. Closed comedones, or whiteheads, can contain trapped bacteria which feed on skin oil and break it down to release a range of free fatty acids and inflammatory chemicals. In some people, this inflammation spreads to involve surrounding tissues, which may partly be an allergic reaction. White blood cells rush into the area to attack the bacteria and release powerful immune chemicals which make the inflammation worse. This can lead to pustules (superficial microabscesses) and papules – raised pimples over a deeper, underlying infection. If not treated, nodules, cysts and scarring can result.
Professional blackhead removers and whitehead extractors are available but must be used gently and carefully. Don’t dig into the skin or you can cause damage and scarring.
The simplest removers are strips that you moisten and apply to the skin. These ‘glue’ themselves to blackheads and extract them when the strip is removed – highly satisfying! Suction devices are also a better, safer option than surgical steel extractors.
Teens and adults get acne
The word acne comes from the Greek word acme meaning prime of life, as it is mainly a condition of youth. But although acne is often viewed as a teenage problem, the number of adults with acne is increasing. As many as 54% of women and 45% of men over the age of 25 show some degree of facial acne, with 12% of women having clinically significant acne until at least their mid 40s.
Around eighty per cent of teens with significant acne are male. Among adults, however, the ratio is reversed and eighty per cent of those affected are female. In both cases, the same underlying cause is an increased sensitivity to male (androgen) hormones.
The best acne treatments
 The three main aims of acne treatment are:
The three main aims of acne treatment are:
- To limit the duration and severity of symptoms
- To reduce the psychological distress that accompanies the condition
- To prevent scarring.
Acne should always be taken seriously and treated properly as scarring can result from all grades of acne, even mild cases and, once formed, scars are permanent although they do fade with time.
Follow instructions, as some treatments work best when applied over the entire affected area, such as the whole face, while others are designed to be applied just on solitary spots.
Be patient. Any new treatment will usually take several weeks to have its full effect, and it is common not to notice any obvious benefits for 6 to 8 weeks after starting therapy. This is how long it can take to ‘reset’ your immune responses involved in triggering acne inflammation. Some treatment may make symptoms worse in the short-term, as they open your pores, before your acne improves.
Do keep up with treatments however, as after two months of continued and regular use, improvements of around 20% per month are common. Treatment is usually needed for at least six months.
Washes for acne
Soap substitutes are useful for cleansing the skin, removing excess grease and maintaining the correct level of skin acidity. These do not irritate the skin and are less drying than soap. Some are mildly antiseptic.
Modern products remove dead skin cells, kill bacteria, eliminate excess oil and reduce redness.
Abrasive agents (eg aluminium oxide, polyethylene granules) in detergent or soaps help to remove excess sebum and comedones and reduce the number of bacterial colonies on the skin. They are suitable for use in mild acne. They can irritate the eyes and skin, however.
Benzoyl peroxide for acne
Benzoyl peroxide has been used for over a hundred years and is still classed by the World Health Organisation as an essential medicine for the skin. Benzoyl peroxide has an antibacterial action against Propionibacterium acnes and can reduce the number of surface bacteria on the skin by 100 fold. Benzoyl peroxide also reduces the number of size of comedones and damps down inflammation, so that the number of size of inflammatory nodules is reduced.
Benzoyl peroxide is applied as a cream, lotion or gel, once per day. Regular use of benzoyl peroxide can reduce acne lesions by 60% after two months treatment, with continuing improvement with continued use.
Start with a lower concentration (2.5% or 5% ) and, if necessary, work up to the 10% products.
Side effects of benzoyl peroxide
Around 40% of people using benzoyl peroxide notice redness and scaling of their skin after the first few days of treatment. But this effect is a part of its action and generally settles down after a couple of weeks. If irritation is excessive, decrease the strength of solution used, and the frequency of application, and apply a non-comedogenic (non-blackhead forming) moisturiser.
Benzoyl peroxide will bleach hair and clothes, so if you are treating your back or chest, wear an old T-shirt under your clothes. When using benzoyl peroxide on your face at night, use an old white pillowcase – don’t use your best bedding.
If you are using prescribed treatments such as tretinoin, you can alternate this with benzoyl peroxide, using one in the morning and the other in the evening (follow your doctor’s instructions). Benzoyl peroxide may also be used with aqueous solutions of topical antibiotics, but not with those in alcohol solutions.
In the US, benzoyl peroxide is available without a pharmacy consultation, but in the UK it is only available from pharmacies, such as Boots.com at the discretion of a pharmacist.
| Acnecide Wash 5% gel (50g) is available from Boots.com. Apply twice a day by wetting your face, then applying the gel. Leave on your skin for 1 to 2 minutes before rinsing off with water. |  |
| Acnecide 5% gel (30g) is available from Boots.com
After washing with a mild cleanser and water, apply Acnecide 5 gel once or twice a day to the entire affected area. |
 |
You can also obtain benzoyl peroxide, benzoyl peroxide with clindamycin antibiotic gel from an on-line consultation with a registered GP via Pharmacy2U.
Azelaic acid for acne
Azelaic acid is produced from oleic acid – the main monounsaturated fat found in olive oil. Despite its innocuous sounding source, it is a powerful anti-acne treatment that is included in many prescription-only medicines for acne and rosacea.
Azelaic acid works in both comedonal acne and inflammatory acne. When applied as a cream, once or twice per day, it kills acne bacteria and decreases the formation of keratin plugs that block oil ducts to reduce comedone formation.
It is as effective as benzoyl peroxide and is a useful alternative if you do not tolerate benzoyl peroxide as it is less drying. Side effects include mild, transient redness and irritation in 5-10% of users. Some azelaic acid solutions are available over-the-counter, but stronger preparations require a prescription.
Nicotinamide gel for acne
Nicotinamide is a form of vitamin B3 which helps to damp down acne inflammation. Applied sparingly once or twice a day as a gel, it reduces inflammation but has no effect on bacteria or blackheads. It is therefore used to treat acne that is predominantly inflammatory rather than comedonal (with blackheads).
A study involving 80 people with moderate inflammatory facial acne compared the effects of nicotinamide gel (4%) with an antibiotic gel (1% clindamycin). After twice daily use of the nicotinamide gel, acne severity grade decreased from an average of 5.9 to 4 after one month with nicotinamide gel, and further reduced to a severity score of 2 after eight weeks. In those using the antibiotic gel, acne severity reduced from an average of 5.7 to 3.85 after one month, and further reduced to a score of 2 after eight weeks.
The treatments were therefore equally successful after two months, but nicotinamide gel has the advantage of being available without a prescription and without the risk of bacterial resistance developing. Nicotinamide gel was also significantly more effective in people with oily skin than clindamycin gel.
Salicylic acid for acne
Salicylic acid solution is related to aspirin and has an anti-inflammatory and drying, exfoliating effect. When applied two or three times a day, it helps to peel off dead skin cells as well as having an antibacterial action.
Salicylic acid can cause irritation and dryness. If you experience irritation, decrease the strength/amount of solution used, the frequency of application, and apply a non-comedogenic (non-blackhead forming) moisturiser.
Salicylic acid is often combined with tea tree oil for an additional, synergistic, antibacterial action.
Tea tree oil for acne
Tea tree oil is an essential oil extracted from a plant native to Australia and has been used as a topical antiseptic treatment for skin infections for hundreds of years. A clinical trial that assessed the effectiveness of a 5% tea tree oil gel in mild to moderate acne in 60 people showed excellent results. In those who used the tea tree ol gel for 45 days, tea tree oil gel was 3.55 times more effective than placebo in getting rid of spots (total acne lesion count) and tea tree oil gel was also 5.75 times more effective than placebo in reducing acne severity.
Another study found that a 5% tea tree oil gel worked as well as 5% benzoyl peroxide in controlling the symptoms of acne, with both treatments having an equal effect in reducing the number of inflamed and non-inflmaed lesions (open and closed comedones). Although the tea tree oil was slower to work than the benzoyl peroxide, it produced fewed side effects and patients generally preferred the tea tree oil gel.
Light therapy for acne
One of the latest hospital treatments for acne is laser therapy, which targets bacteria deep within the oil glands. Similar therapies are now available for home use. These produce specific wavelengths of red and blue light which both kill the skin bacteria that trigger spots, and damp down inflammation.
Blue and red light phototherapy has been shown to reduce the number of acne lesions by 46% after 4 weeks daily treatment, and by 81% after 12 weeks. Researchers at the Imperial College of Science Technology and Medicine concluded that phototherapy with mixed blue-red light is an effective treatment for mild to moderate acne, with no significant side effects.
Light treatments can be used alone or in combination with other treatments to combat acne. Some are pen-sized to target individual spots, while others treat the whole face.
Treatments typically take between 15 and 30 minutes per day. If safety glasses are provided, always use these. Some masks can be worn while doing homework, watching TV or reading, as part of your daily lifestyle.
Diet and acne
There is increasing evidence that diet plays a significant role in triggering the inflammation associated with acne. A high intake of sugar and refined carbohydrates (eg white flour products, processed cereals) increases circulating levels of both a substance called insulin-like growth factor which, in turn, increases the activity of oil-producing glands, and the proliferation of sticky skin cells which block your pores.
Click here to read more about the link between diet and acne.
Click here to read how chocolate can make acne worse.
And if all else fails, here are my favourite spot zappers – keep one in your pocket for when a pimple starts to emerge. The earlier a blemish is treated, the quicker it will resolve.
When to see your doctor
Treatments can take 8 weeks or more to work, so persevere. If you don’t notice any improvement, or if your skin starts to flare up and you can’t control it with over-the-counter products, consult your doctor. Acne must be treated effectively to prevent permanent scarring.
First line treatments are usually topical creams, lotions and gels such as benzoyl peroxide or azelaic acid (which kill bacteria and reduce blackheads). If you’ve already used these, let your doctor know so they can prescribe stronger versions, and consider whether or not to prescribe topical antibiotics.
Topical antibiotics for acne
Your doctor may prescribe antibiotic lotions for moderate acne that mainly affects the face. These solutions may contain erythromycin (plus or minus zinc acetate) or clindamycin and are applied twice daily to reduce the numbers of bacteria on the skin. They have a similar overall efficacy to benzoyl peroxide, but some Propionibacterium acnes infections are becoming resistant.
Combining topical antibiotic treatment with benzoyl peroxide reduces bacterial resistance to treatment.
Topical antibiotics are also available combined with tretinoin or isotretinoin – forms of vitamin A.
Side effects: Topical antibiotics are less irritant than benzoyl peroxide. One or two preparations fluoresce under ultraviolet light, however, so don’t put use them before going to a disco.
Oral antibiotics for acne
Oral antibiotic treatments may be prescribed for mild to moderate acne that affects a large area such as the face, back and chest. Studies show they reduce the number of Propionibacterium acnes bacteria on the skin by around tenfold. If there is no improvement after 3 months, the antibiotic should be changed. Maximum improvement is usually seen after 4 – 6 months, but in severe cases, treatment may need to be continued for two years or more.
There is a move away from using oral antibiotics, because bacterial resistance is an increasing problem.
Side effects: Long term use of antibiotics affects bacterial balance in the gut and can lead to oral thrush, nausea, abdominal pain or diarrhoea in around 5% of people.
If oral antibiotics are needed, a probiotic supplement containing probiotic bacteria will help to reduce intestinal side effects.
Anti-androgens for acne
A synthetic hormone, cyproterone acetate, which blocks the effects of male hormones, can be used in females as both an acne treatment and oral contraceptive Pill for women also requiring contraception. It is prescribed in combination with oestrogen (co-cyprindiol) and is licensed for use in women with moderate to severe acne that has not responded to topical therapy or oral antibiotics. It also improves moderately severe hirsutism (excess body hair) and it beneficial for women with polycystic ovary syndrome (PCOS).
Your doctor will inform you that there is an increased risk of develoing blood clots (venous thromboembolism) when using co-cyprindiol, particularly during the first year of use. The risk of a blood clot is around 1.5 to 2 times higher than in women using combined oral contraceptive pills containing levonorgestrel. Whether this is due to the medication or to the increased underlying risk associated with the underlying hormone imbalance is not clear.
Vitamin A derivatives for acne
Tretinoin, isotretinoin and adapalene are vitamin-A like medicines which are applied as a cream or gel, once or twice daily, for a minimum of two months. They work by stimulating division of fibroblast cells deep in the skin. This proliferation helps push spots up and out, to such an extent that initially, skin may appear worse – lumpy and inflamed – before improving. They also reduce the number of sticky skin cells within hair follicles, allowing blocked comedones to empty and restore the free flow of sebum. Tretinoin and isotretinoin are used when comedones, papules and pustules predominate. The majority of users show a 70% response over three to six months of treatment.
Side effects: Excessive use results in thin, shiny, red skin with soreness and peeling. There may be occasional photoirritation with ultraviolet light.
Oral isotretinoin (also an analogue of vitamin A) is only prescribed by hospital specialists and has revolutionised the treatment of severe acne. As it is toxic, it is usually reserved for patients with severe cystic acne, and for those who have not responded to several courses of antibiotics because of bacterial resistance.
Isotretinoin capsules are taken once or twice per day for 1 to 4 months and repeat courses are not normally recommended. Isotretinoin works by reducing sebum secretion which, in turn, prevents comedone formation and damps down inflammation. It is so effective that sebaceous follicles shrink significantly within two weeks of regular treatment, and the amount of sebum secreted rapidly falls. Isotretinoin does not have an antibiotic action, but reduces the number of Propionibacterium acnes bacteria on the skin by suppressing the production of sebum on which they ‘feed’.
Side effects of isotretinoin treatment are common, with facial redness in two-thirds of users, conjunctivitis in a third, eczema in a third Muscle and joint aches, headache and dry mucous membranes, cracked lips and nose bleeds can also occur, as can raised blood levels of cholesterol and triglycerides. Some people also experience severe depression although this has not been definitely linked to isotretinoin use.
Monthly blood tests and supervision are necessary throughout therapy. It is only used in women of child-bearing age if they are using an effective method of contraception and register with a pregnancy prevention program, as it can cause fetal abnormalities.
Despite this long list of possible complications, treatment under close specialist supervision can transform the quality of life for people with severe acne.
Cosmetic treatment for acne scars
Cosmetic treatments are excellent for treating acne scars, which are of three main types:
– Superficial, violet-coloured, ice-pick scars (small pits)
– Thick, palpable scars from deeper lesions
– Thickened (keloid) scars which tend to occur on the shoulders, chest and back.
Cosmetic treatments include skin peeling agents, skin abrasives, laser therapy and collagen injections to plump up and even out pits. Collagen injections need repeating every six months or so.
Alternatively, cysts and scars may be surgically removed or injected with steroids.
Which acne treatments have you found most effective? Please share your experience via the comment box below.
Image credits: pixabay

My 14yr old was plagued with face & back acne. We tried all the washes, topical treatments & even invested in a light therapy mask for £50. Age 16 we asked for an appointment with the dermatology department at the hospital. Took 6 months to get one in Lincolnshire. By this time her face looked like it was scarring & was starting to pop up on her neck too. She did her best with make up & avoided oily cosmetics, washed the brushes regularly.
Oh and her GP even put her on the mini pill for three months, that didn’t help one bit.
Dermatologist prescribed oral Isotretanoin after a blood test to check kidney function. Within 7 days there was a miraculous change in her face. She had to continuously apply lip balm and after two months start wearing hand cream, red patches of dry skin on her hands & wrist. The Isotretanoin dries the skin up, her hair only needed washing to freshen it up, it didn’t get greasy. After three months & beautiful skin the concentration was increased by the dermatologist, which surprised me, she was given the maximum dose.
I’m happy to report she’s been medication free for nearly four months and still hasn’t had any spots, there’s no scarring. The pores on her face are still smaller but the oils in her hair is probably a more normal level.
Yippee, my girl looks lovely & is so happy.
Her sister age 14 is starting to look similar, back & chest spots and her face is a mess. we tried acnecide this week but her cheeks have swollen up. Here we go again!
Hi Jo, Really glad the isotretinoin worked. Acne causes such emotional turmoil at a very sensitive time in life. Great news. Sarah B